Depression isnt a choice its a kind of brain damage – Depression isn’t a choice; it’s a kind of brain damage. This isn’t about weakness or a lack of willpower; it’s about a complex interplay of biological, psychological, and social factors. Understanding these factors is crucial for recognizing the condition, offering support, and advocating for effective treatments. This exploration delves into the scientific understanding of depression, highlighting the biological underpinnings, psychological influences, and social contexts that contribute to its manifestation.
We’ll also examine the implications for treatment and support, ensuring a comprehensive perspective.
The idea that depression is a medical condition, not a character flaw, has significantly evolved over time. Early perceptions often viewed it as a sign of personal failing, leading to stigma and hindering appropriate support. However, modern research underscores the biological basis of depression, emphasizing the role of neurochemical imbalances, genetics, and brain structure in its development. Furthermore, psychological factors, such as stress, trauma, and learned helplessness, play a critical role in the experience of depression.
Understanding the Statement
The statement “depression isn’t a choice; it’s a kind of brain damage” highlights a crucial shift in how we understand and treat depression. It moves away from blaming individuals for their condition and towards recognizing it as a complex medical issue with biological underpinnings. This perspective emphasizes the importance of seeking professional help and support for those struggling with depression, fostering a more compassionate and understanding environment.This statement acknowledges the significant biological factors contributing to depression, challenging the notion that it’s simply a matter of willpower or personal weakness.
Instead, it frames depression as a consequence of dysregulation in the brain, comparable to other medical conditions like diabetes or heart disease. This understanding is crucial for effective treatment and reduces the stigma often associated with mental illness.
Biological Perspectives on Depression
Depression is increasingly recognized as a complex disorder involving intricate interactions between biological, psychological, and social factors. A significant biological component involves neurotransmitter imbalances, particularly in the levels of serotonin, dopamine, and norepinephrine. Research suggests that genetic predisposition plays a role in vulnerability to depression, meaning certain individuals may be more susceptible to developing the condition due to their inherited genetic makeup.
Furthermore, structural and functional differences in the brain, such as reduced hippocampal volume or altered activity in specific brain regions, have been observed in individuals with depression.
Psychological Perspectives on Depression
Psychological factors, such as stressful life events, coping mechanisms, and personality traits, also significantly contribute to the development and progression of depression. Early childhood experiences and the accumulation of significant stressors can increase an individual’s vulnerability to depression. Cognitive distortions, or negative thought patterns, are often implicated in the maintenance of depressive symptoms. Psychological therapies, such as cognitive behavioral therapy (CBT), aim to address these psychological factors to alleviate symptoms.
Social Perspectives on Depression
Social factors, including social support networks, socioeconomic status, and cultural norms, also play a critical role in the experience of depression. Individuals with strong social support systems tend to cope better with stress and maintain mental well-being. Conversely, isolation, discrimination, and societal pressures can contribute to the development and perpetuation of depressive symptoms.
Understanding depression as a kind of brain damage, rather than a personal failing, is crucial. It’s not a choice, and it’s often surprisingly similar to the challenges faced by parents of ADHD children, who frequently experience a deep empathy for the struggles of their kids. For example, 15 things parents of ADHD children understand well highlight this shared experience of navigating complex neurological conditions.
Ultimately, acknowledging the biological basis of depression is key to proper support and treatment, just as understanding the neurological underpinnings of ADHD is essential for effective parenting.
Brain Damage in Mental Health
The term “brain damage” in the context of mental health refers not to physical trauma or injury to the brain but to functional or structural changes in the brain. These changes can be subtle and may not always be immediately apparent through physical examination. Neurological disorders like Parkinson’s disease or multiple sclerosis involve significant physical damage to the brain, which is distinct from the functional alterations observed in depression.
Neurochemical imbalances and structural variations within the brain, linked to depression, are better understood as forms of brain
- dysregulation* rather than
- damage* in the conventional sense.
The Evolution of Depression as a Medical Condition
Historically, depression was often viewed as a character flaw or a sign of personal weakness. However, advancements in neuroscience and psychiatry have progressively shifted the understanding of depression toward a more medical model. The development of effective medications, such as selective serotonin reuptake inhibitors (SSRIs), and the recognition of the biological basis of depression have been instrumental in this evolution.
Furthermore, the increasing emphasis on mental health awareness and support has led to a greater acceptance of depression as a treatable medical condition.
Biological Basis of Depression
Depression, a pervasive mental health condition, isn’t simply a matter of willpower or a character flaw. It’s a complex disorder rooted in biological mechanisms, primarily involving imbalances in brain chemistry and structure. Understanding these biological underpinnings is crucial for developing effective treatments and fostering empathy for those affected. This exploration delves into the neurochemical imbalances, brain structures, genetic predispositions, and imaging techniques that contribute to our understanding of depression.
Neurochemical Imbalances
Neurotransmitters are chemical messengers in the brain that facilitate communication between nerve cells. Imbalances in these crucial chemicals can significantly impact mood regulation. The following table illustrates some key neurotransmitters and their potential roles in depression:
| Neurotransmitter | Function | Imbalance (Potential in Depression) | Symptoms |
|---|---|---|---|
| Serotonin | Regulates mood, appetite, sleep, and other bodily functions. | Reduced levels or impaired function. | Sadness, anxiety, difficulty concentrating, sleep disturbances, changes in appetite. |
| Dopamine | Plays a role in motivation, reward, pleasure, and movement. | Reduced levels or impaired function. | Loss of interest, decreased motivation, fatigue, difficulty experiencing pleasure. |
| Norepinephrine | Influences alertness, arousal, and stress response. | Reduced levels or impaired function. | Fatigue, difficulty concentrating, low energy levels, slowed movements. |
| GABA (Gamma-aminobutyric acid) | Inhibits neuronal activity, promoting relaxation and calming effects. | Reduced levels or impaired function. | Anxiety, irritability, difficulty sleeping, heightened stress response. |
Brain Structures Implicated in Mood Regulation
Several brain structures are critical for mood regulation, and dysfunction in these areas can contribute to depression. These structures include:
- Amygdala: This almond-shaped structure processes emotions, particularly fear and anxiety. Overactivity in the amygdala, potentially linked to sustained stress, may contribute to heightened negative emotions.
- Hippocampus: This seahorse-shaped structure plays a role in memory formation, particularly of emotional experiences. Reduced volume or function of the hippocampus has been observed in individuals with depression, potentially affecting memory and emotional processing.
- Prefrontal Cortex: This area is crucial for higher-level cognitive functions like decision-making, planning, and emotional regulation. Dysfunction in the prefrontal cortex has been linked to difficulties with emotional control and decision-making, which can manifest as symptoms of depression.
- Anterior Cingulate Cortex: This brain region is involved in error detection, conflict resolution, and regulating emotions. Dysfunction in this area might lead to difficulties managing negative emotions and experiences.
Genetic Vulnerability
Genetic predisposition plays a significant role in vulnerability to depression. Research indicates that individuals with a family history of depression are at a higher risk. This doesn’t mean a certain gene directly causes depression, but rather that specific genetic variations can increase the susceptibility to developing the disorder.
Brain Structure and Function
Neuroimaging studies have revealed structural and functional differences in the brains of individuals with depression. For example, reduced gray matter volume in specific brain regions, such as the hippocampus, has been associated with depression. These structural changes may correlate with functional alterations, such as impaired communication between different brain regions, further impacting mood regulation.
Brain Imaging Techniques
Several brain imaging techniques are used to study depression. These include:
- Magnetic Resonance Imaging (MRI): This technique provides detailed structural images of the brain, allowing researchers to assess the volume and morphology of different brain regions. MRI scans are used to look for structural differences, like changes in brain volume or shape, associated with depression.
- Functional Magnetic Resonance Imaging (fMRI): This technique measures brain activity by detecting changes in blood flow. fMRI scans help identify areas of the brain that are more or less active during specific tasks or emotional states, offering insights into functional abnormalities related to depression.
- Positron Emission Tomography (PET): This technique uses radioactive tracers to visualize brain activity. PET scans can measure neurotransmitter activity and receptor binding, providing information about neurochemical imbalances in the brain, which can help understand depression.
Psychological Factors in Depression
Depression isn’t simply a chemical imbalance; it’s a complex interplay of biological, psychological, and social factors. Understanding the psychological dimensions of depression is crucial for effective treatment and management. This involves exploring the diverse range of thoughts, feelings, and behaviors that contribute to the condition, from cognitive distortions to the impact of adverse life events.Psychological theories of depression offer valuable insights into the mechanisms underlying the disorder.
These perspectives, including cognitive, behavioral, and psychodynamic approaches, provide different lenses through which to examine the experience of depression, emphasizing different contributing factors. By considering these diverse viewpoints, we can gain a more comprehensive understanding of the condition and develop more effective interventions.
Different Psychological Theories of Depression
Various psychological theories attempt to explain the development and maintenance of depression. Cognitive theories highlight the role of negative thought patterns and distorted thinking in contributing to depressive symptoms. Behavioral theories focus on learned responses and environmental factors, such as reinforcement and punishment, in shaping depressive behaviors. Psychodynamic theories emphasize the influence of unconscious conflicts and past experiences on current emotional states.
Each perspective offers unique insights into the complex nature of depression.
It’s crucial to remember that depression isn’t a choice; it’s a genuine neurological condition, a type of brain damage. Understanding this can be a first step towards healing. Learning to connect with your inner self is vital for navigating challenges like depression. Exploring methods to improve self-awareness and productivity, like the ones outlined in this article on 5 ways to connect with your inner self and increase productivity 5 ways to connect with your inner self and increase productivity , can offer a pathway towards better mental well-being.
Ultimately, recognizing depression as a health issue is key to recovery and building resilience.
Role of Stress, Trauma, and Adverse Childhood Experiences
Stressful life events, trauma, and adverse childhood experiences (ACEs) can significantly increase the risk of developing depression. Experiences such as abuse, neglect, loss, or significant adversity can create lasting emotional wounds and contribute to maladaptive coping mechanisms. These experiences can shape an individual’s vulnerability to future stressors and their ability to regulate emotions. Trauma, in particular, can disrupt the individual’s sense of safety and security, leading to long-term emotional dysregulation.
Individuals with a history of trauma may exhibit heightened anxiety, difficulty regulating emotions, and an increased risk of depression.
Learned Helplessness and Negative Thought Patterns
Learned helplessness, a concept developed by Martin Seligman, posits that individuals who repeatedly experience uncontrollable negative events may develop a sense of hopelessness and a belief that their efforts will not affect outcomes. This learned helplessness can manifest as a passive attitude and a diminished motivation to cope with challenges. Negative thought patterns, including catastrophizing, all-or-nothing thinking, and overgeneralization, contribute significantly to depressive symptoms.
These patterns can lead to a distorted view of oneself, the world, and the future, perpetuating feelings of sadness and hopelessness.
Coping Mechanisms and Resilience
Developing effective coping mechanisms is essential for managing depression. These mechanisms can involve strategies such as stress reduction techniques, problem-solving skills, and social support networks. Resilience, the ability to bounce back from adversity, plays a critical role in preventing and mitigating the impact of depression. Resilient individuals possess a set of strengths, such as optimism, a sense of control, and strong social connections, which enable them to navigate stressful situations more effectively.
Comparison of Psychological Therapies for Depression
| Therapy Type | Principles | Techniques | Effectiveness |
|---|---|---|---|
| Cognitive Behavioral Therapy (CBT) | Focuses on identifying and modifying negative thought patterns and maladaptive behaviors. | Cognitive restructuring, behavioral activation, exposure therapy. | Generally considered highly effective in treating mild to moderate depression. Studies show significant improvements in mood and functioning. |
| Psychodynamic Therapy | Examines the unconscious motivations and past experiences that contribute to current psychological distress. | Free association, dream analysis, transference interpretation. | Can be effective for individuals with more severe or chronic depression, particularly when combined with other approaches. May require a longer treatment duration. |
| Interpersonal Therapy (IPT) | Addresses interpersonal problems and social difficulties that may contribute to or worsen depressive symptoms. | Communication skills training, problem-solving techniques, relationship enhancement. | Demonstrates efficacy in treating depression, especially when social factors play a significant role in the individual’s experience. |
| Acceptance and Commitment Therapy (ACT) | Focuses on accepting difficult thoughts and feelings while committing to valued actions. | Mindfulness exercises, acceptance strategies, values clarification. | Shows promise in treating depression, particularly in reducing emotional distress and increasing psychological flexibility. |
Social and Environmental Factors
Depression isn’t confined to the brain alone; its roots often intertwine with the social and environmental tapestry of a person’s life. Understanding these external influences is crucial for effective treatment and prevention. Social support, societal stigma, socioeconomic factors, and cultural norms all play a significant role in shaping the experience and outcome of depression. Recognizing these multifaceted interactions is essential for a comprehensive approach to mental health.
Influence of Social Support Systems
Social support, encompassing the emotional, practical, and informational assistance provided by others, is a powerful buffer against depression. Strong social networks provide individuals with a sense of belonging, encouragement, and practical help during challenging times. This support can manifest in various forms, from listening ears and comforting words to tangible assistance like childcare or financial aid. Individuals with robust social support systems often demonstrate greater resilience and quicker recovery from depressive episodes.
Conversely, a lack of social connection can increase vulnerability to depression. Studies consistently demonstrate a correlation between strong social support and lower rates of depression.
Societal Stigma and Discrimination
Societal stigma surrounding mental illness, including depression, often creates a significant barrier to seeking help. The fear of judgment, discrimination, and social exclusion can prevent individuals from admitting their struggles or seeking appropriate treatment. This stigma manifests in various ways, from subtle biases in interpersonal interactions to overt discrimination in employment or housing. The negative perception of mental illness can lead to isolation and self-stigma, further exacerbating the individual’s suffering.
This often leads to delayed treatment, hindering recovery and potentially prolonging the course of the illness.
Socioeconomic Factors
Socioeconomic factors, including poverty and limited access to resources, are strongly correlated with increased rates of depression. Poverty often creates significant stress and instability, impacting various aspects of daily life, from housing and food security to access to healthcare and education. These stressors can negatively affect mental well-being and contribute to the development of depression. Lack of access to quality healthcare and mental health services further compounds the problem.
Individuals facing financial hardship and limited resources are often unable to afford or access the support they need, leading to a vicious cycle of disadvantage and poor mental health.
Cultural Beliefs and Norms
Cultural beliefs and norms significantly influence how depression is expressed and experienced. Different cultures have varying understandings of mental illness, which can impact how individuals perceive and articulate their emotional distress. Some cultures may discourage the expression of negative emotions, while others may attribute mental health issues to supernatural causes. These cultural differences can influence help-seeking behaviors and treatment adherence.
Furthermore, cultural norms surrounding gender roles, family expectations, and social obligations can contribute to increased vulnerability to depression for certain groups within a society.
Correlation Between Social Factors and Depression Rates
| Demographic | Social Factors | Depression Rate | Contributing Factors |
|---|---|---|---|
| Low-income individuals | Poverty, limited access to resources, financial stress | Higher | Increased stress, lack of social support, limited access to healthcare |
| Individuals with limited social support | Lack of strong social networks, isolation | Higher | Decreased resilience, difficulty coping with stressors |
| Marginalized groups (e.g., LGBTQ+ individuals, racial minorities) | Societal stigma, discrimination, prejudice | Higher | Increased stress, fear of judgment, limited access to resources |
| Individuals from cultures with limited mental health awareness | Cultural beliefs and norms that discourage the expression of emotions | Potentially Higher (depending on cultural context) | Delayed help-seeking, misdiagnosis, lack of cultural sensitivity in treatment |
Implications for Treatment and Support: Depression Isnt A Choice Its A Kind Of Brain Damage
Depression is a complex illness, and effective treatment requires a multifaceted approach that acknowledges its biological, psychological, and social dimensions. Early intervention and a personalized treatment plan are crucial for successful management and recovery. This section will delve into the importance of early intervention, explore available treatment options, emphasize the need for patient-centered care, and Artikel the ongoing support required for individuals struggling with depression.
Importance of Early Intervention and Diagnosis
Early identification and diagnosis of depression are paramount. The sooner treatment begins, the more effective it is likely to be, minimizing the severity of symptoms and preventing potential long-term consequences. Prompt intervention can also prevent the development of associated conditions, such as anxiety disorders or substance abuse. Early diagnosis allows for the implementation of targeted therapies and supports, facilitating a faster recovery and improved quality of life.
Available Treatment Options
A range of treatment options are available for depression, and the most effective approach is often a combination of strategies tailored to the individual’s needs. These include medication, therapy, and lifestyle modifications.
Medication
Medication plays a significant role in managing depression. Antidepressants work by altering the levels of neurochemicals in the brain, such as serotonin and norepinephrine, which are associated with mood regulation. Different types of antidepressants target specific neurotransmitter systems, leading to varied effectiveness and side effect profiles. The choice of medication is often determined through consultation with a mental health professional, considering the individual’s specific symptoms and medical history.
Therapy
Psychotherapy, or talk therapy, is another crucial component of depression treatment. Different types of therapy, including cognitive behavioral therapy (CBT), interpersonal therapy (IPT), and psychodynamic therapy, can help individuals understand and manage their depressive symptoms. These therapies equip individuals with coping mechanisms and strategies to address underlying emotional issues and develop healthier thought patterns.
Okay, so, depression isn’t a choice; it’s a real, biological thing, a kind of brain damage. It’s tough, and it’s important to remember that. But, even when you’re feeling down in your 30s, there are still signs you might be thriving, even if you don’t feel it. Check out this list of 10 signs you’re thriving in your 30s, even if you don’t feel like you are to see if maybe you’re doing better than you think.
Ultimately, understanding that depression is a health issue, not a character flaw, is key. It’s crucial to remember that.
Lifestyle Changes
Lifestyle changes can significantly impact the management of depression. Regular exercise, a balanced diet, sufficient sleep, and stress reduction techniques can all contribute to improved mood and overall well-being. These lifestyle adjustments are not only beneficial for depression but also for overall health and wellness.
Patient-Centered Care
Patient-centered care is essential in managing depression. This approach prioritizes the individual’s unique experiences, preferences, and values in the treatment process. Open communication, shared decision-making, and a strong therapeutic alliance are vital for successful outcomes. This individualized approach allows for a more effective and supportive treatment experience.
Types of Medications Used in Treating Depression, Depression isnt a choice its a kind of brain damage
| Medication Type | Mechanism of Action | Potential Side Effects | Effectiveness |
|---|---|---|---|
| Selective Serotonin Reuptake Inhibitors (SSRIs) | Block the reuptake of serotonin, increasing its availability in the synapse. | Nausea, insomnia, sexual dysfunction, weight changes. | Generally effective for mild to moderate depression. |
| Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) | Block the reuptake of both serotonin and norepinephrine. | Nausea, headache, insomnia, sexual dysfunction. | Often effective for moderate to severe depression. |
| Tricyclic Antidepressants (TCAs) | Block the reuptake of norepinephrine and serotonin, and affect other neurotransmitters. | Dry mouth, constipation, blurred vision, weight gain. | Effective, but typically reserved for cases where SSRIs or SNRIs are not suitable. |
| Monoamine Oxidase Inhibitors (MAOIs) | Inhibit the enzyme monoamine oxidase, preventing the breakdown of neurotransmitters. | Significant dietary restrictions, potential for dangerous interactions with certain foods and medications. | Effective for specific types of depression, but often not the first choice due to safety concerns. |
Ongoing Support and Resources
Continued support and access to resources are crucial for individuals recovering from depression. This includes ongoing therapy sessions, support groups, and access to educational materials. Connecting with others who understand the challenges of depression can provide invaluable emotional support and practical advice. Maintaining a strong support system, whether through family, friends, or professional resources, is vital for long-term well-being.
Illustrative Cases and Examples
Understanding the multifaceted nature of depression requires looking at real-life examples. Each person’s experience is unique, shaped by a complex interplay of biological predispositions, psychological factors, and social circumstances. This section explores illustrative cases to highlight the diversity and complexity of this challenging condition.
A Case Study: Sarah’s Journey
“Depression is like a relentless storm, brewing within and battering against me from all sides.” – Sarah
Sarah, a 32-year-old marketing executive, experienced a gradual decline in mood over several months. Initially, she attributed her fatigue and lack of motivation to stress at work. However, the symptoms persisted and worsened, affecting her sleep, appetite, and concentration. Her social life suffered as she withdrew from friends and family. Physiological symptoms such as headaches and digestive problems emerged.
Genetic predisposition played a role, as her mother had a history of anxiety and mood disorders. Chronic stress from a demanding job and a strained relationship with her partner further contributed to her experience. Therapy helped Sarah identify negative thought patterns and develop coping mechanisms. Medication provided support by regulating neurotransmitter levels, allowing her to participate in social activities and gradually regain a sense of normalcy.
This case illustrates the intricate interplay of biological, psychological, and social factors in depression. The severity of her symptoms and their duration underscore the importance of early intervention and professional support.
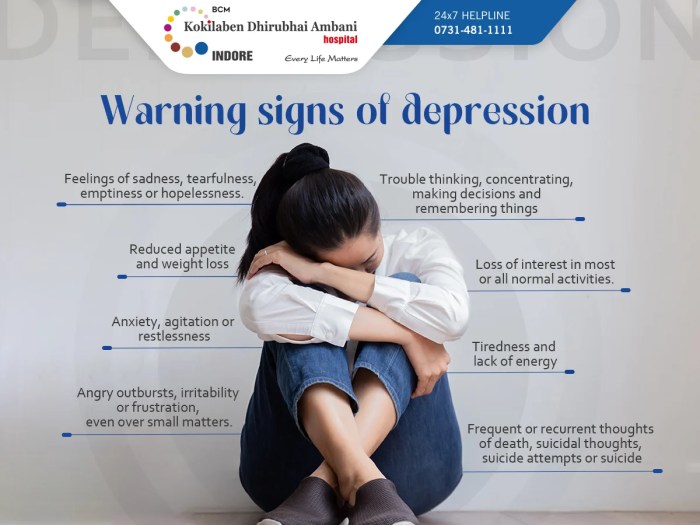
Diverse Experiences of Depression
Depression manifests in various ways, impacting individuals differently in terms of severity and presentation. Some experience significant sadness and hopelessness, while others may primarily exhibit irritability, anger, or a loss of interest in activities they once enjoyed. Some individuals may experience physical symptoms, such as chronic pain or fatigue, while others primarily struggle with emotional and cognitive difficulties.
The diversity in presentation emphasizes the importance of individualized assessment and treatment approaches. A comprehensive understanding of the individual’s experience is crucial for effective support and intervention.
A Fictional Case: Emily’s Story
“I feel like I’m drowning in a sea of negativity, with no way to reach the surface.” – Emily
Emily, a 20-year-old college student, felt increasingly overwhelmed by the pressures of academics and social expectations. Her anxieties grew, manifesting as racing thoughts, difficulty concentrating, and persistent feelings of inadequacy. Social isolation became a pattern, as she avoided interactions with peers and withdrew from campus activities. Her sleep was severely affected, and her appetite fluctuated wildly. Emily’s feelings of hopelessness intensified, and she struggled to maintain a sense of purpose.
She struggled with a fear of failure and perfectionism, which compounded her feelings of worthlessness. Her experience highlights the significant impact of social and environmental factors on the development and manifestation of depression. Her journey underscores the need for empathetic support and understanding from friends, family, and mental health professionals. The importance of creating a safe space for individuals experiencing these struggles cannot be overstated.
The Importance of Empathy and Understanding
Empathy and understanding are essential in supporting individuals experiencing depression. Recognizing the individual’s unique experience, acknowledging the complexity of the condition, and providing non-judgmental support are critical. Creating a safe and supportive environment allows individuals to open up about their struggles and seek professional help. A crucial element of support is patience and acceptance. Individuals experiencing depression may not always be forthcoming or responsive.
Building a supportive network and encouraging open communication is paramount to recovery. Understanding that depression is not a personal failing, but a complex medical condition, is essential for fostering empathy and reducing stigma.
Final Conclusion
In conclusion, depression isn’t a choice; it’s a complex condition stemming from a multitude of interconnected factors. Recognizing the biological, psychological, and social aspects is paramount to providing effective support and treatment. Understanding that depression is a medical condition, not a personal failing, is crucial in breaking down stigma and fostering a compassionate approach to those affected. By acknowledging the intricate nature of depression, we can work towards creating a more supportive and understanding environment for those struggling.